Respiratory Infections (Overview)

Most of the time, respiratory infections during pregnancy resemble infections in non-pregnant women. They go away on their own with time and without the use of antibiotics or other prescription medications.
While there is very limited information regarding how pregnancy alters the course of respiratory infections, it does not appear that women are more susceptible to infection overall, but they may be more vulnerable to severe illness after contracting specific infections (i.e. influenza).
To date, management of most of these illnesses during pregnancy remains the same as the general population. However, earlier diagnosis is preferable to avoid any potential complications (i.e. pneumonia) and avoidance of unnecessary antibiotics.
Therefore, pregnant women are advised to call their HCP if they are experiencing respiratory illness, especially if fever is present or they have an underlying respiratory or cardiac condition. Women are also advised to call their HCP or seek emergency care if they experience shortness of breath, chest pain, and/or severe cough.
Detailed information regarding COVID-19 and pregnancy can be read here.
*Women experiencing trouble breathing or extreme shortness of breath should seek emergency medical care immediately or dial 911*
Background
Common colds, which are caused by different types of viruses that can affect the upper and/or lower respiratory tracts, are very common and behave similarly in pregnant women as they do in non-pregnant women.
Upper respiratory tract: nose, pharynx and larynx
Lower respiratory tract: trachea, bronchi, bronchioles, alveolar duct and alveoli
Upper respiratory infection is the most commonly reported infection during pregnancy, with an estimated 49.6% of women in the United States (U.S.) being affected at some point just prior to pregnancy or during pregnancy.
Most of these infections go away on their own with supportive care and over-the-counter (OTC) medications. However, sometimes the infection spreads to other nearby organs, leading to possible complications such as pneumonia.
Infections can be caused by viruses or bacteria, but most are viral. Viruses are also the most common causes of sinus infections and bronchitis.
Although most viruses that cause "common colds" have not been identified, some of the known viruses that cause respiratory infections include:
Rhinovirus (most common in pregnant women; no vaccine, no treatment – over 100 different types)
Influenza (vaccine, antiviral medications in limited circumstances)
COVID-19 (coronavirus; no vaccine, no proven treatment)
Respiratory Syncytial Virus (RSV) (no vaccine, preventive treatment in high risk infants/children)
Human metapneumovirus (hMPV)
Enterovirus
Adenovirus
Respiratory infections are highly contagious. Viruses can be caught through direct person-to-person contact, contaminated surfaces (fomites), or through the air (aerosol); the virus usually enters an individual through the eyes, nose, or mouth (i.e. “don’t touch your face").
In one study, rhinovirus was detected on 40% of patients’ hands (i.e. "wash your hands").
In a separate study, rhinovirus was transmitted through the air by the mouth (breathing) to 10 of 18 volunteers who played cards for several hours with infected individuals (i.e social distancing).
Viral Respiratory Infections and Pregnancy (Overview)
Pregnancy-specific changes to the body can make fighting off and managing respiratory symptoms more difficult compared to prior to pregnancy.
Several viral upper respiratory infections are known to have a more severe course during pregnancy. Because most of pregnancy can be considered an anti-inflammatory state, women who contract viral infections requiring an inflammatory response tend to get more severe infections (the inflammation necessary to fight the infection is delayed). However, this also depends on stage of pregnancy and type of virus.
The increase in progesterone in pregnancy causes the nasal capillaries, nasal mucosa, and upper respiratory tract to swell; this helps viruses attach and makes it harder for immune cells in the nasal cavity to kill these pathogens.
Along with upper respiratory tract swelling, lung expansion is restricted as the uterus enlarges; this can lead to a greater need for intensive care and mechanical ventilation during pregnancy in case of severe respiratory virus infection.
NOTE: Pregnant women do not have weaker immune systems than non-pregnant individuals; their immune systems are just "different". Learn more about this here.

Symptoms
Symptoms such as fever, cough, nasal stuffiness/congestion, sneezing, runny nose, and sore throat are all common symptoms of a respiratory infection that can be produced in different combinations depending on the virus. Symptoms usually resolve without treatment within 7 to 10 days, but coughing can persist for much longer in some cases.
Coughing, and the mechanisms by which viruses cause coughing is still not understood, and some viruses can produce worse cough than others. Fortunately, there is no evidence that coughing, even when severe, can cause complications during pregnancy. While there are no effective cough medications that can cure a viral-induced cough, over-the-counter medications can help suppress a cough until the virus runs its course.
Any pregnant woman with an unrelenting cough needs to call her HCP to rule out other causes and prevent possible further illness. Women should never take OTC cough medication without first speaking with their HCP.
Fever is a common sign/symptom of a respiratory infection, but may not be present in mild infections. Women are advised to call their HCP any time they experience a fever (at least 100.4° F/38° C). High, prolonged fever has been associated with negative outcomes during pregnancy.
Nasal congestion is also a common symptom of respiratory infection, as well as pregnancy in general. Women can experience nasal congestion as a result of viral or bacterial infection – which usually occurs with other symptoms – or congestion due to pregnancy, which usually presents on its own.

Rhinovirus
Rhinovirus is the most common cause of respiratory infections in pregnant women and the general population (up to 80%) and can infect the upper and lower respiratory tracts* (*less common). Rhinovirus infections occur year-round with seasonal peaks between September and November, and again from March to May.
Symptoms include runny nose, nasal congestion, sore throat, cough, headache, and fever.
Rhinovirus infection can make individuals more susceptible to follow-on bacterial infections (such as ear and sinus infections), and those with asthma can develop more serious illness. There are no anti-viral drugs that are effective against rhinovirus.
Influenza
Influenza ("flu") is a common respiratory infection around the world, and it is often indicated that pregnant women may experience more severe illness. In the United States, influenza season normally begins in October and can last until May each year.
Symptoms of influenza include fever, muscle and joint pain, headache, dry cough, runny nose, nasal congestion, and extreme fatigue.
However, influenza infection, and its prognosis during pregnancy on both mother and baby, appears to depend upon:
Severity of infection
Stage of pregnancy
Underlying illnesses
Vaccination status
Overall health of the pregnancy
When the woman sees an HCP or receives medical care

Not all pregnant women who contract influenza will have serious illness. However, there is currently no way to determine which women may experience a more severe course of the disease. Therefore, the earlier a woman is seen, tested, diagnosed, and treated, the better the prognosis.
Current research indicates, to date, the best way women can protect themselves and their babies during pregnancy is to practice good hygiene, get vaccinated, and call their HCP immediately when they have a fever or believe they may have influenza (read more).
COVID-19
According to currently available case series and cohorts as of October 2021, data indicates pregnant women are not more susceptible to contracting COVID-19 than non-pregnant women, and fetal and symptomatic neonatal infection appear to be rare events.
However, pregnant women who contract COVID-19 appear to be at higher risk of certain complications from the disease than non-pregnant women of reproductive age. These complications include Intensive Care Unit admission, mechanical ventilation, and the need for extracorporeal membrane oxygenation (ECMO), as well as the risk of death (although overall risk remains low).
Read COVID-19 and Pregnancy for more detailed information, to include COVID-19 vaccine safety data.

Respiratory Syncytial Virus (RSV)
Adults – including pregnant women – can contract RSV. Based on common thought that RSV infects only young children, RSV is not often tested in pregnant women; therefore, very little is known about the infection during pregnancy.
Symptoms of RSV in adults include cough, runny nose, and congestion.
There are case reports of RSV-related complications during pregnancy, but the prevalence of this is unknown since routine screening for this virus is not common. However, rapid testing is now available which allows for earlier and more specific diagnosis.
Because the true prevalence is not yet known, adverse outcomes can only be loosely linked. It does appear, however, that misdiagnosis is common, asthma may play a role in severe infection, and overall, there may be an increased risk of pneumonia and/or preterm delivery.
“Despite the potential for devastating consequences, RSV infection in pregnant [individuals] has likely been unrecognized… With the increased availability of [testing], we suspect that we are now recognizing an infection that has long been present..."
RSV infection during pregnancy may adversely affect the fetus, but more research is necessary:
The first (and recent) animal studies of this kind indicate RSV infection can cross the placenta and potentially harm the developing immune system and/or lungs of the fetus (especially early in pregnancy).
These complications during gestation were shown to weaken the ability of the offspring to fight against RSV exposure after birth.
Although almost all research to date has been in animal studies (human studies of this nature are not ethical), the first human case of vertical transmission (infection from pregnant woman to fetus) was just recently reported (2017) in which the baby was born with RSV and had symptoms; the virus has also been found in human cord blood in numerous cases.
Although current data indicates this is rare, this entire field is relatively new, this has never been specifically studied, and therefore the true prevalence of RSV vertical transmission is not known.
Pregnant women with a respiratory infection can ask to be tested for RSV (along with strep, influenza, and/or COVID-19). RSV testing is now inexpensive and readily available. Further, testing could prevent misdiagnosis and inappropriate use of antibiotic drugs, and may result in faster treatment with oxygen and/or possible antiviral medications.
RSV is a major cause of serious and potentially fatal respiratory infection in infants and toddlers. As no preventable vaccine is currently available, a vaccine for mothers during pregnancy is being developed with the purpose of passing antibodies to the baby to prevent the number of infants/young children with severe forms of this illness.
Human Metapneumovirus (HMPV)
HMPV is a respiratory virus that commonly mimics RSV; it can cause severe lower respiratory tract disease (primarily in children); there is very little information on HMPV during pregnancy as the virus itself was only discovered in 2001.
HMPV is estimated to cause 1.5% to 10.5% of respiratory infections among adults, but could account for up to 15% of all hospitalizations related to respiratory infections.
In one of the first major studies of HMPV in pregnant women, it was found to be four times more common, with symptoms lasted slightly longer than pregnant women with RSV. However, pregnant women with HMPV and postpartum women with HMPV had a similar experience/prognosis, indicating that pregnancy may not make HMPV infection more severe, but more research is needed.

Enterovirus
Enteroviruses are also a cause of respiratory infections but are usually very mild unless the infection spreads to the central nervous system. Types of enteroviruses include non-polio enterovirus infections, coxsackievirus (hand, foot, and mouth), hepatitis A and B, and poliovirus.
General symptoms may include fever, mild respiratory symptoms, muscle aches, rash, and gastrointestinal symptoms. Infections usually spread in summer and fall.
Enteroviruses are not studied often during pregnancy, but reported cases during pregnancy have been documented. One study indicated that of all pregnant women studied with an unexplained fever, almost 12% were determined to have an enterovirus.
Fortunately, although data is incomplete, an enterovirus infection during pregnancy does not readily appear to transfer to the fetus; further, it is assessed that most newborns of infected mothers will have no illness or experience any negative outcome.
Currently, based on a lack of data, there is no information regarding recommendations for diagnosis, screening, or management of these infections during pregnancy, although RT-PCR testing is available.
In 2014, the U.S. experienced a dramatic increase in EV-D68, which caused severe respiratory illness, mostly in children.
Interestingly, the first 2014 confirmed case of severe respiratory tract infection in an adult from EV-D68 occurred in a pregnant woman. Although her infection was severe, she had a normal, uneventful vaginal delivery and fully recovered.
CDC recommends that HCPs consider testing for enteroviruses when any individual presents with severe respiratory illness with an unclear cause.
Adenovirus
Adenoviruses are very contagious and common viruses that normally produce respiratory infections (bronchitis, pneumonia) or conjunctivitis (pink eye) at any time during the year, in both children and adults.
Infection is normally mild unless an individual has an existing respiratory or cardiac disease. Severe maternal infection during pregnancy has been reported, but it is considered very rare.
Symptoms include cough, fever, fast breathing, wheezing, sore throat, and diarrhea.
Despite a lack of data, adenovirus has been detected in the placenta and amniotic fluid. Further, one study noted that adenovirus was the most common viral pathogen identified in fetal samples from pregnancies with amniotic fluid abnormalities. However, the significance of this is not known and more research is necessary.
Although no specific treatment exists, HCPs can perform testing to identify a cause of an unknown severe respiratory infection. Management is considered supportive, which indicates rest, fluids, and possible OTC medications (after discussion with an HCP).

Bacterial Respiratory Infections (Overview)
The most common bacterial respiratory infections during pregnancy include sinus infections (sinusitis; see Sinus Infection section, below) and pneumonia.
S. pneumoniae, H. influenzae and Moraxella catarrhalis are responsible for a large percentage of these infections.
Pneumonia
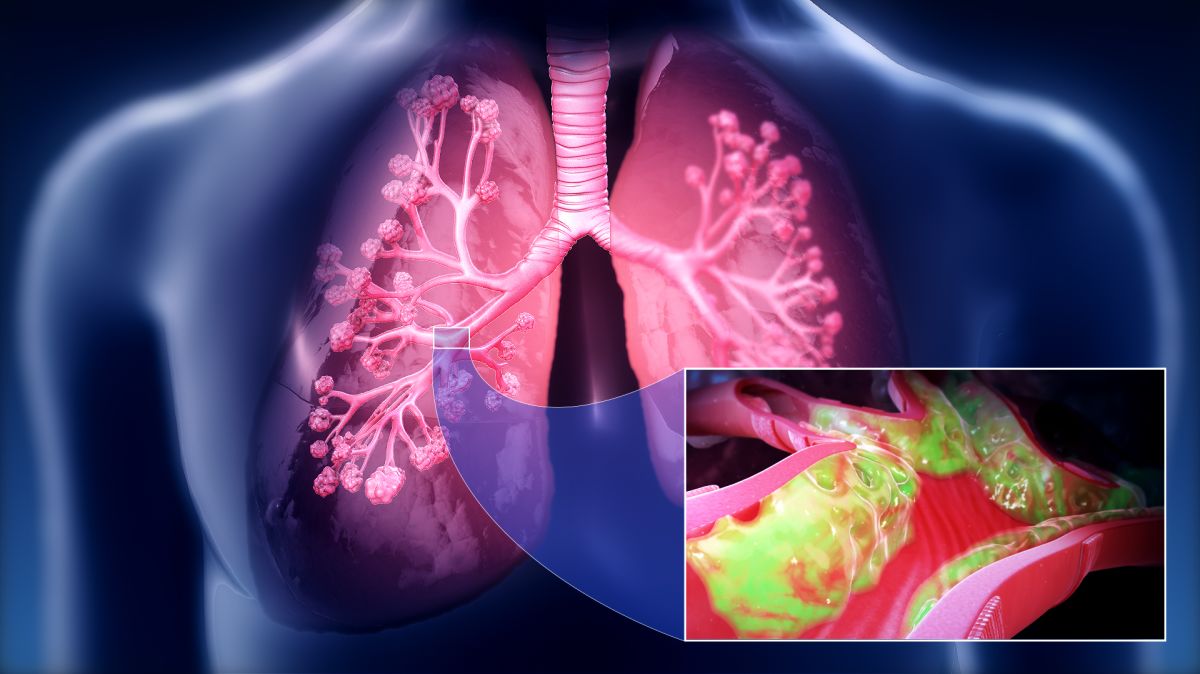
Pneumonia can be viral or bacterial. Viral pneumonia usually occurs secondary to a primary viral infection, such as influenza. Bacterial pneumonia is due to a bacterial infection of the air sacs and surrounding tissue in the lung(s) which causes significant inflammation and fluid build up (see image below).
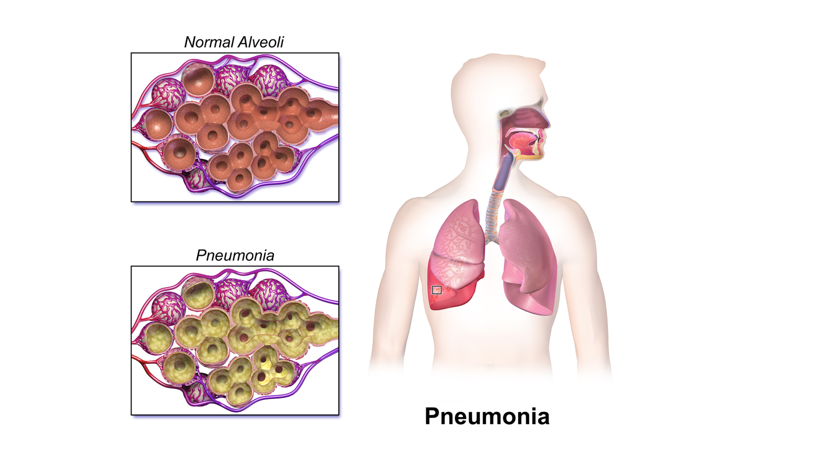
Symptoms of bacterial pneumonia can include include fever, cough, chest pain, rigors, chills, and shortness of breath. With viral pneumonia, symptoms may have a more gradual onset and fever is general lower than with bacterial pneumonia.
Pneumonia is the most frequent cause of fatal non-obstetric infection during pregnancy, but is still considered relatively uncommon (0.5 to 1.5 per 1,000 pregnancies in the U.S.). It is assessed that respiratory, immune, and cardiac system changes of pregnancy may make pneumonia more severe and difficult to treat than in non-pregnant women, but studies remain inconsistent.
Regardless, underlying diseases such as asthma and anemia appear to increase the risk of contracting pneumonia in pregnancy.
Preterm birth and possible transmission of the infection to the newborn is possible. To prevent these negative outcomes, early diagnosis and treatment (antibiotics) is critical. It is often recommended that pregnant women with severe respiratory illness should receive a chest x-ray to prevent any delay in pneumonia diagnosis. Women should have a risks and benefits discussion with their HCP regarding any medical imaging during pregnancy.
Sinus Infection (Rhinosinusitis)
Along with common colds, sinus infections are one of the most common infections in the general population and affect millions of adults in the U.S. each year. Despite the common belief that sinus infections require antibiotics, the viruses described above are the most common cause.
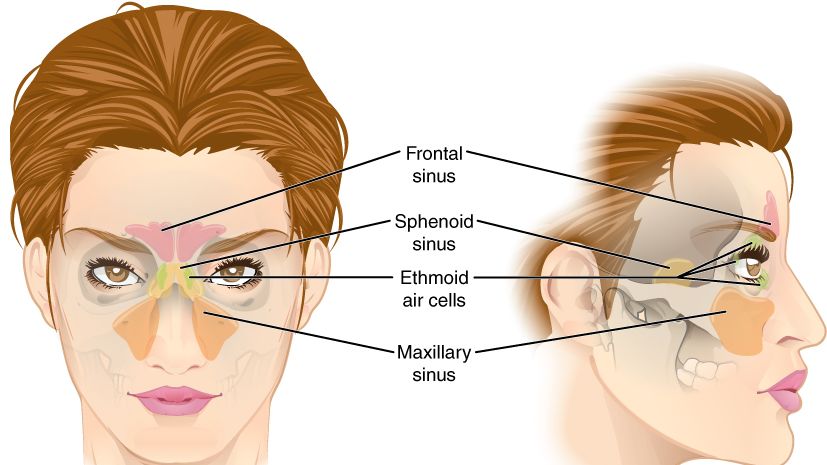
Sinusitis (or rhinosinusitis) affects about 1 in 8 adults annually and occurs when viruses (or bacteria/fungi) infect the sinuses (usually during a cold) and begin to reproduce. The nasal cavity/sinus lining swells as a reaction to the infection, blocking the channels that drain the sinuses which causes mucus to fill the cavities.
The sinuses are a group of hollow spaces that surround the nose and are also found above and between the eyes; these cavities connect to the nose through small, narrow channels. The sinuses are healthy when the channels are open, allowing air through and drainage out.
Symptoms of a sinus infection during pregnancy are similar to those who are not pregnant, but the congestion and pain can be made worse/compounded by the general nasal congestion that pregnancy causes by itself, without an infection (read Nasal Congestion).
Sinus infections may include symptoms such as cloudy or colored nasal drainage with nasal blockage or clogging, facial pain/pressure, or both. Other symptoms include fever, cough, fatigue, diminished sense of smell, tooth pain, and ear fullness/congestion (the latter can also be made worse through pregnancy-associated fluid changes).
The biggest difference between a viral sinus infection and a bacterial sinus infection is that a viral infection usually improves within 10 days and does not progressively get worse, while a bacterial infection will get worse and last longer (or gets worse after a period of getting better); an acute bacterial sinus infection can last as long as four weeks.
Good, quality evidence and official guidance regarding the management of sinus infections during pregnancy is lacking, despite the major effect on a pregnant woman’s quality of life – especially with a lengthy infection and near constant nasal congestion.
Furthermore, as of 2015, clinical practice guidelines on chronic sinus infection from the American Academy of Otolaryngology-Head & Neck Surgery and the European Rhinologic Society did not offer structured guidelines to HCPs on managing sinus infections in pregnant women.
Therefore, management is similar to non-pregnant individuals, which includes OTC medications for pain and discomfort, and antibiotics if the infection is assessed by an HCP to be bacterial.
Management
The management of severe colds, sinus infections, and more serious respiratory infections require discussions between pregnant women and their HCPs regarding the risks and benefits of diagnosis, management, and treatment.
Mild respiratory infections generally go away on their own within 7 to 10 days. Viral infections cannot be treated with antibiotics, therefore women can use symptom-reducing lifestyle modifications or OTC medications until the infection runs its course.
Women who are assessed to have a bacterial respiratory/sinus infection may be prescribed an antibiotic. Women should follow all guidelines and instructions regarding any prescription medication as indicated by their HCP.
Action
Pregnant women are advised to call their HCP if they are experiencing respiratory illness, especially if fever is present or they have an underlying respiratory or cardiac condition.
Women are also advised to call 911 or seek emergent medical attention if they are experiencing chest pain, shortness of breath, trouble breathing, and/or have a severe, unrelenting cough.
More detailed information regarding COVID-19 and pregnancy can be found here.
Women can read more about the safety of various OTC cold medications here.
Women should also consider sharing and submitting an experience (below) related to having a respiratory infection during pregnancy (influenza, COVID-19, bronchitis, pneumonia).
Women can feel anxious with any symptoms that could resemble influenza or COVID-19. Hearing from other pregnant women can relieve anxiety and help them be better advocates for themselves.
Resources
The Management of Respiratory Infections During Pregnancy (Immunology and Allergy Clinics of North America; 2006)
Adenovirus Fact Sheet (American Thoracic Society, 2019)
COVID-19 Home Page (U.S. Centers for Disease Control and Prevention)
COVID-19 FAQs for Obstetrician-Gynecologists, Obstetrics (American College of Obstetricians and Gynecologists)
Assessment and Treatment of Pregnant Women With Suspected or Confirmed Influenza (American College of Obstetricians and Gynecologists)